
Written by Parmin Sedigh
Illustrated by Maggie Huang
and Sabrina Chen
Cancer is universally feared—and for good reason. It’s the cause of death for one in four Canadians.¹ In our fight against cancer, we’ve taken a two-pronged approach: diagnose cancer earlier through screening, and research new medications and surgeries to treat cancer more effectively upon diagnosis. Over the past three decades, the five-year survival rate from all cancers has increased by over 10% in Canada, due in no small part to screening.¹
There’s no doubt about it: screening has saved countless lives. Yet, the fear of cancer continues to grip society. In other words, our societal perception of cancer has been trailing behind our immense scientific progress in both treatments and screening—a fear that American surgeon George Crile Jr. called “cancerphobia” back in 1955.
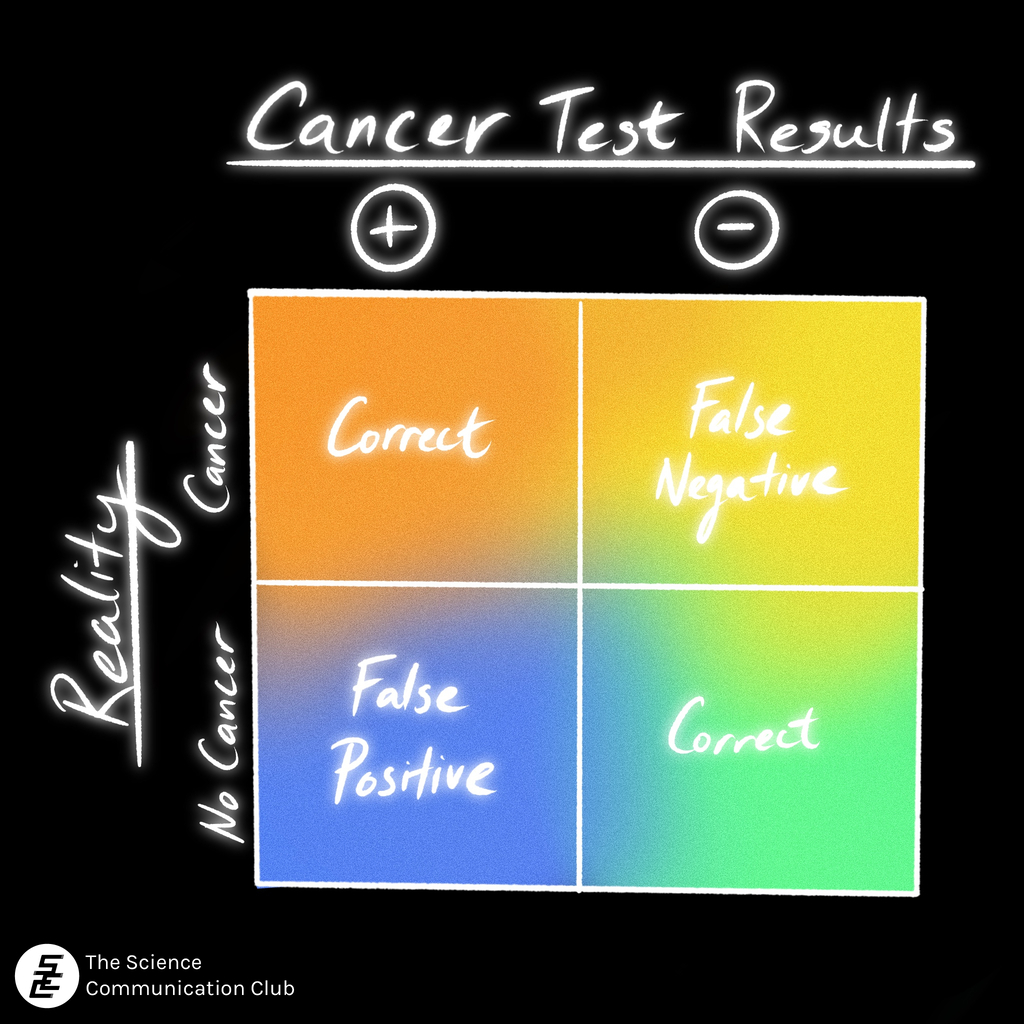
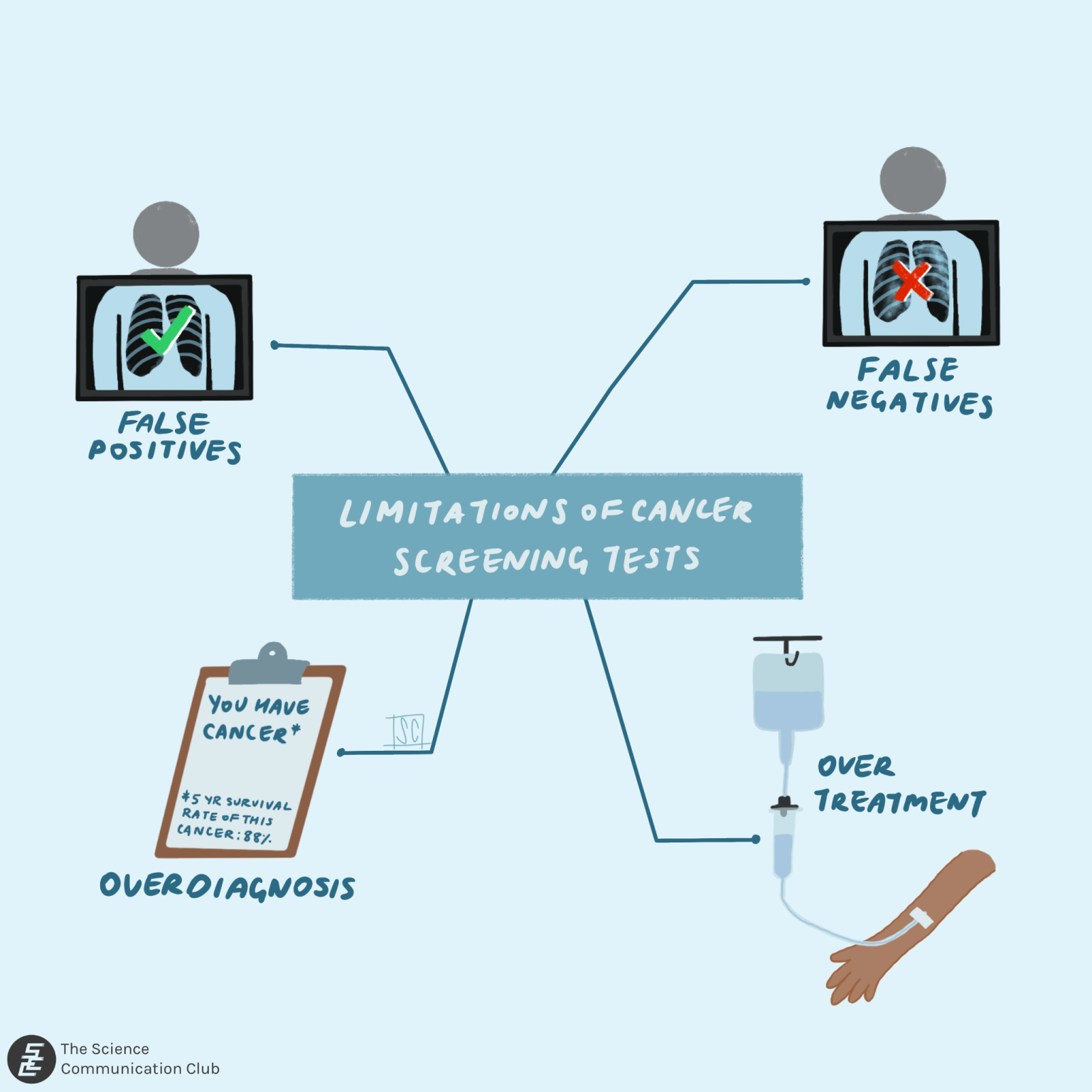
The Canadian Cancer Society lists four main buckets of the limitations of cancer screening tests: testing positive when the patient doesn’t truly have cancer (false positives), testing negative when the patient does have cancer (false negatives), diagnosing cancers that would likely not lead to death or adverse effects had they gone undiagnosed (overdiagnosis), and adding subsequent tests or treatments that may not have been necessary (overtreatment).² (This list may have been inspired by Ned Calonge’s approach to thinking about screening limitations.³) The first two buckets are scientific problems—issues with the screening technology. The latter two buckets are social or communication problems and are the ones we’ll focus on.
When it comes to overdiagnosis and overtreatment, cancerphobia can play a big role and has for decades now. For instance, a 1959 Canadian Gallup public opinion poll asked the following questions: “What disease do you think kills the most people in this country?” and “Is there any disease you think about a lot? If yes, which one?”. 52.5% of respondents correctly said that heart disease kills the most people,⁴ followed by 44.3% who said it’s cancer.⁵ But when it came to which disease people thought about a lot, 39.6% mentioned cancer. Heart disease was mentioned by only 6.4% of respondents.⁴
While this disconnect between the biggest killer and the most feared disease doesn’t necessarily mean that people would opt for unnecessary screening, more recent surveys suggest that this is indeed the case. A study of 1,580 Americans found that one-third of participants were willing to undergo screening tests even when explicitly told that they could cause harm (due to subsequent unnecessary treatments) and did not decrease deaths.⁶
There are many reasons for this fear. For one, we tend to leave all mathematical reasoning behind when faced with a scary possibility. Researchers at Harvard University asked students how much they were willing to pay to rid the water supply of arsenic that could cause cancer (described using emotional and gruesome language). The amount of money they were willing to pay was essentially the same for both participant groups, one of which was told the risk of cancer was 1 in 100,000 while the other was told the risk was 1 in a million.⁷ Additionally, as David Ropeik writes in Curing Cancerphobia: How Risk, Fear, and Worry Mislead Us, the fear of regret can be a large factor. No one wants to be diagnosed with cancer years after having chosen not to undergo screening, only to wonder how things could have been different. Ropeik also mentions other contributors such as the common perception that dying of cancer is much more painful and prolonged than dying of other diseases, and wanting the ability to take control of our lives and fates through screening, among other reasons.⁸
But is overdiagnosis and overtreatment really that big of a problem? Researchers at Dartmouth College estimated that one-quarter of breast cancers found through mammography screening and six-in-ten prostate cancers found through the prostate-specific antigen test may have been overdiagnosed—meaning the cancer would never have progressed further, or would have progressed slowly enough for the patient to have died of another cause.⁹
So how do we combat this? The Dartmouth researchers suggest increasing the positivity thresholds for screening tests as one approach, though this method can lead to controversy and confusion among both patients and physicians. One method is to better educate patients about the limits of screening, especially if a patient is asking for screening outside of the recommended guidelines. Medical professionals could also benefit from more awareness of the problem of overdiagnosis and overscreening. Incorporating information about proper screening that balances the benefits and harms into medical school curricula would be a good start.⁹
Importantly, despite the dangers of overscreening, underscreening for certain cancers can be just as problematic, if not more so. For example, the relatively new lung cancer screening test (which uses low-dose CT scans) is not widely adopted in the US or Canada. In the US, a 2015 report estimated that less than 5% of those eligible for screening received the test.¹⁰ In Canada, there are fully implemented lung cancer screening programs in only two provinces—British Columbia and Ontario—as of 2022.¹¹ This is in contrast to other screening programs such as those for breast cancer, which exist in all provinces and territories, with the exception of Nunavut.¹²
To be clear, this article isn’t meant to discourage you from getting screened. If your physician recommends a screening test, or if you receive a screening test in the mail, please get the test. It can not only save your life but also make your treatment more comfortable and effective. If you ever suspect something is wrong, please consult a doctor. Trust yourself and don’t ignore any signs.
But it’s also good to keep this quote by French philosopher Paul Virilio in mind when it comes to any technological or scientific advancement: “The invention of the ship was also the invention of the shipwreck.” There’s no way to make a perfect cancer screening test or program, but greater awareness of the dangers of overdiagnosis might help us prevent shipwrecks as much as possible.
Sources:
- Canadian Cancer Statistics Advisory Committee in collaboration with the Canadian Cancer Society, Statistics Canada and the Public Health Agency of Canada. Canadian Cancer Statistics 2023. 2023. cancer.ca/Canadian-Cancer-Statistics-2023-EN
- Canadian Cancer Society. Benefits and limitations of regular cancer screening. Canadian Cancer Society. [accessed 2024 Mar 23]. https://cancer.ca/en/cancer-information/find-cancer-early/screening-for-cancer/benefits-and-limitations-of-regular-cancer-screening
- Ned Calonge – The Challenge of Communicating Overdiagnosis. 2015. https://www.youtube.com/watch?v=9jA_WWAxrmo
- Gallup Canada, 2019, “Canadian Gallup Poll, May 1959, #275”, https://doi.org/10.5683/SP2/931AEW, Borealis, V1, UNF:6:b+ccuKbuv5bGIsaZ54ZqtA== [fileUNF]
- Dominion Bureau of Statistics. Fatal Accidents Mortality Summary 1959. 1961. https://publications.gc.ca/collections/collection_2018/statcan/CS84-513-1961-eng.pdf
- Scherer LD, Valentine KD, Patel N, Baker SG, Fagerlin A. A bias for action in cancer screening? Journal of Experimental Psychology. Applied. 2019;25(2):149–161. doi:10.1037/xap0000177
- Sunstein CR, Zeckhauser R. Overreaction to Fearsome Risks. Environmental and Resource Economics. 2011;48(3):435–449. doi:10.1007/s10640-010-9449-3
- Ropeik D. Curing Cancerphobia: How Risk, Fear, and Worry Mislead Us. Johns Hopkins University Press; 2023.
- Welch HG, Black WC. Overdiagnosis in cancer. Journal of the National Cancer Institute. 2010;102(9):605–613. doi:10.1093/jnci/djq099
- National Cancer Institute. Lung Cancer Screening. 2023. https://progressreport.cancer.gov/detection/lung_cancer
- Canadian Partnership Against Cancer. Lung cancer screening in Canada: 2021/2022. 2022. https://www.partnershipagainstcancer.ca/topics/lung-cancer-screening-in-canada-2021-2022/programs/
- Canadian Cancer Society. How do I find a breast cancer screening program? https://cancer.ca/en/cancer-information/find-cancer-early/get-screened-for-breast-cancer/how-do-i-find-a-breast-cancer-screening-program