Written by Ian Yang
Illustrated by Amy Jiao
Patients who suffer from accidents such as extensive burns are typically inflicted with deep skin wounds which have potentially caused heavy damage to their skin layers. In such a case, split-thickness skin grafting is typically employed, where healthy donor skin is grafted into the surface layer and part of the underlying layers of the damaged skin. Unfortunately, skin grafting on large wounds requires a large amount of healthy donor skin to cover all skin layers, which is rarely available. The large wound would only be partially grafted, leaving a portion of the area uncovered, resulting in poor healing conditions.
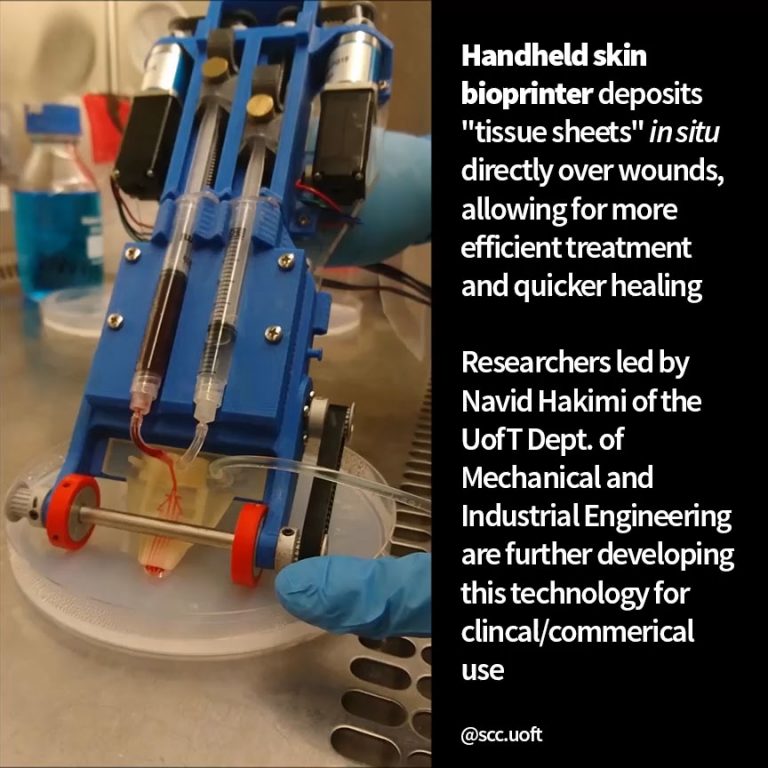
A team of researchers led by PhD student Navid Hakimi of the Department of Mechanical and Industrial Engineering at the University of Toronto have developed a handheld 3D skin printer that is capable of depositing layers of skin tissue to cover and heal deep wounds. It is the first device of its kind that is capable of synthesizing and depositing skin tissue at the location of the wound within two minutes or less. The printer resembles a larger version of a white-out tape dispenser, but with a microdevice that forms skin tissue sheets instead of the tape roll. The current version of the printer device is reported to be the size of a small shoe box, weighs less than a kilogram, and requires minimal operator training to use the device, making it extremely portable and accessible.
More importantly, the device eliminates the additional steps post tissue synthesis and application that are typically required for most conventional bioprinters. The team plans to broaden the capabilities of the printer, particularly by expanding the size of the possible wound treatment area. Alongside Dr. Mark Jeschke’s team at Sunnybrook Hospital, Hakimi’s team plans to perform more studies in live models to further improve the printer’s development. Perhaps one day we will be able to “white out” our burn wounds with this device!
Sources:
- Hakimi, Navid, et al. “Handheld Skin Printer: in Situ Formation of Planar Biomaterials and Tissues.” Lab on a Chip, vol. 18, no. 10, 2018, pp. 1440–1451., doi:10.1039/c7lc01236e.